When you suffer a stroke, seconds count. Early treatment can lead to higher survival rates and lower chance of severe disability. Fortunately, our stroke team offers highly specialized expertise and advanced stroke treatment options.
Hemorrhagic Stroke
Surgery to remove pooled blood from the brain and repair damaged blood vessels is often required for hemorrhagic strokes. The type of surgery depends upon the specific cause of brain bleeding.
One common problem related to brain bleeding is hydrocephalus, which is the build-up of fluid within the brain. A procedure called ventriculostomy may be needed to drain the fluid.
Ischemic Stroke
Thrombolytics, such as tissue plasminogen activator (tPA), may be given if the stroke is caused by a blood clot. This medication breaks up blood clots and helps restore blood flow to the damaged area. Thrombolytics are not given if you are experiencing a hemorrhagic stroke. The medication could cause increased bleeding.
It’s important you are examined and treated by a specialized stroke team within three hours of experiencing symptoms. If the stroke is caused by bleeding rather than clotting, thrombolytics can make the damage worse -- so care is needed to diagnose the cause before any treatment is administered.
The decision to give the drug is based upon:
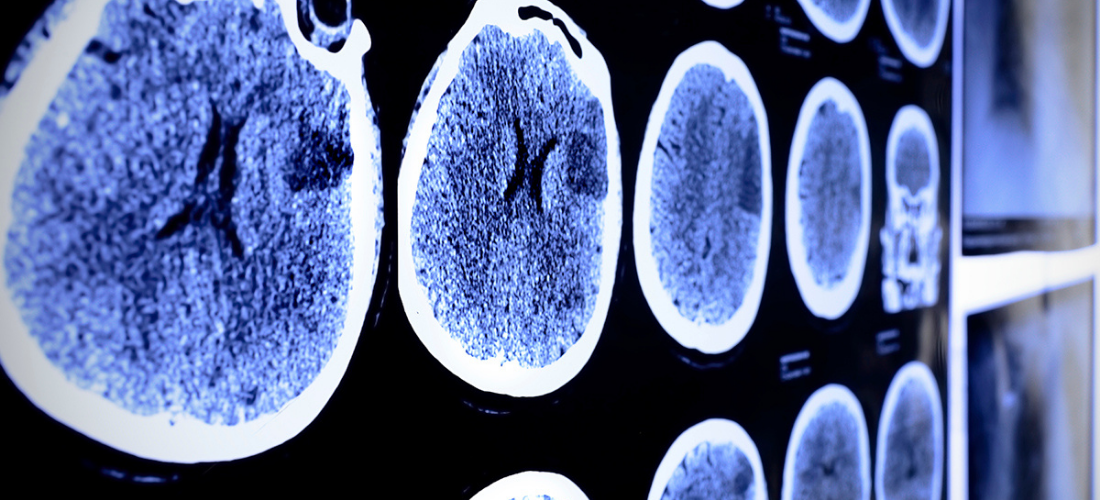
- A brain CT scan to make sure there is no bleeding
- A physical exam that shows a significant stroke
- Your medical history
In other circumstances, blood thinners such as Heparin and Coumadin are used to treat strokes due to blood clots. Aspirin also may be used. Other medications may be needed to control other symptoms, including high blood pressure. Painkillers may be given to control severe headache.
Carotid Artery Surgery
Carotid artery surgery is a procedure to restore proper blood flow to the brain. The build-up of plaque in the inner layer of the wall of an artery may lead to narrowing and irregularity. Where the narrowing is severe, there is a risk that the vessel can block completely if a thrombus (blood clot) forms in the diseased segment.
There are two ways to treat a carotid artery that has plaque buildup in it. One is surgery called endarterectomy. The other is a procedure called angioplasty with stent placement.
Carotid artery surgery may help lower your chance of having a stroke. But you will need to make lifestyle changes to help prevent plaque buildup, blood clots, and other problems in your carotid arteries over time. You may need to change your diet and start an exercise program, if your doctor tells you exercise is safe for you.